Day 3 :
Keynote Forum
Samer Ellahham
Sheikh Khalifa Medical City, UAE & Cleveland Clinic, USA
Keynote: HFpEF: Cardiovascular abnormalities not just comorbidities
Time : 10:45-11:25

Biography:
Samer Ellahham has served as Chief Quality Officer at Shaikh Khalifa Medical City since 2009. In his role, he has led the development of a quality and safety program that has been highly successful and visible and has been recognized internationally by a number of awards. As Chief Quality Officer and Global Leader, he has focus on ensuring that that implementation of this best practices leads to breakthrough improvements in clinical quality and patient safety. He is the recipient of the Quality Leadership Award from the Global Awards for Excellence in Quality and Leadership and the Business Leadership Excellence Award from the World Leadership Congress. He was nominated in 2015 for SafeCare magazine Person of the Year. He is Certified Professional in Healthcare Quality (CPHQ). He is a recognized leader in quality, safety, and the use of robust performance improvement in improving healthcare delivery.
Abstract:
Nearly half of all patients with heart failure have a normal ejection fraction (EF). The prevalence of this syndrome, termed heart failure with preserved ejection fraction (HFpEF), continues to increase likely because of the increasing prevalence of common risk factors, including older age, female gender, hypertension, renal dysfunction, metabolic syndrome and obesity. In contrast to heart failure with reduced ejection fraction (HFrEF), no treatment has been proven in pivotal clinical trials to be effective for HFpEF, largely because of the pathophysiological heterogeneity that exists within the broad spectrum of HFpEF. This syndrome was historically considered to be caused exclusively by left ventricular diastolic dysfunction, but research has identified several other contributory factors, including limitations in left ventricular systolic reserve, systemic and pulmonary vascular function, nitric oxide bioavailability, chronotropic reserve, right heart function, autonomic tone, left atrial function and peripheral impairments. Multiple individual mechanisms frequently coexist within the same patient to cause symptomatic heart failure, but between patients with HFpEF the extent to which each component is operative can differ widely, confounding treatment approaches. Clinical trials have not yet identified effective treatments for HFpEF. Incomplete understanding of the pathophysiology of HFpEF, the likelihood that there is substantial pathophysiologic heterogeneity among affected patients and the interplay of various risk factors has all been barriers in the development of effective treatments. Ongoing research initiatives are critically important as there is a rapid increase in number of patients with this form of heart failure.
Learning Objectives: Objectives are to: Demonstrate the association between heart failure with preserved ejection fraction (HFpEF) and survival; given a patient with heart failure (HF), recognize HFpEF on the basis of clinical signs and symptoms, physical examination, echocardiography, and radiographic findings; classify patients at high risk of hospitalization and mortality through assessing risk factors, clinical presentation and interpretation of biomarkers; distinguish the clinical presentation, diagnosis and treatment strategies of HFpEF from those of HF with reduced ejection fraction; given a patient with HFpEF, develop an individualized treatment plan based on current evidence; assess the potential role of future pharmacotherapies for HFpEF.
- Case Study on Cardiology | Research on Cardiology | Biomarkers and Enzymes for Heart Disease | Obesity and Heart | Cardiac Regeneration and Repair
Location: London, UK

Chair
Annamaria Vianello
Gabriele Monasterio Foundation, Italy
Session Introduction
Samer Ellahham
Sheikh Khalifa Medical City, UAE & Cleveland Clinic, USA
Title: The importance of multidisciplinary approach
Time : 09:30-10:00

Biography:
Samer Ellahham has served as Chief Quality Officer for Sheikh Khalifa Medical City, since 2009. In his role, he has led the development of a quality and safety program that has been highly successful and visible and has been recognized internationally by a number of awards. As Chief Quality Officer and Global Leader, he has focus on “Ensuring that that implementation of this best practices leads to breakthrough improvements in clinical quality and patient safety”. He is the recipient of the Quality Leadership Award from the Global Awards for Excellence in Quality and Leadership and the Business Leadership Excellence Award from the World Leadership Congress. He was nominated in 2015 for SafeCare magazine Person of the Year. He is Certified Professional in Healthcare Quality (CPHQ). He is a recognized leader in quality, safety, and the use of robust performance improvement in improving healthcare delivery.
Abstract:
In most countries worldwide, the number of patients with chronic heart failure (HF) is growing with 1-3% of the adult population suffering from this syndrome, rising to about 10% in the very elderly. In the near future, a large part of the worldwide population will suffer from heart failure and society will be faced with the consequences. On average, one in five patients is readmitted within 12 months, making heart failure one of the most common causes of hospitalization in people over 65 years of age. A multidisciplinary team approach involving several professionals with their own expertise is important in attaining an optimal effect. Physicians, nurses and other health care professionals are keys ensuring the delivery of evidence based care. Markers of clinical (in) stability, psychosocial risk factors, and issues related to patient mobility might be important indicators to determine which inter-professional service might be most effective for which patient. Current HF guidelines recommend that HF patients are enrolled in a multidisciplinary-care management program to reduce the risk of HF hospitalization. A multidisciplinary approach to HF may reduce costs, decrease length of stay, curtail readmissions, improve compliance and reduce mortality. An important limitation, however, is the substantial heterogeneity in both the terms of the models of care and the interventions offered, including: clinic or community-based systems of care, remote management and enhanced patient self-care. Conventional trials that randomize individual patients may not be the best way to test the effect of a service; novel approaches, such as the cluster randomized controlled trial, may be superior. It is unlikely that any one approach is optimal. The best form of care might seek to compensate for the weaknesses of each approach by exploiting their strengths. A strong HF cardiology lead, supported by primary care physicians, nurse specialists and pharmacists in the hospital and community with the ability to offer patients remote support might offer the best service. Key to the success of multidisciplinary HF programs may be the coordination of care along the spectrum of severity of HF and throughout the chain-of-care delivered by the various services within the healthcare system. Further research is warranted to identify the most efficacious multidisciplinary approaches to HF.
Learning Objectives: Objectives are to: Define multidisciplinary approach to HF; examine the literature role and recommendations of multidisciplinary in HF and; identify barriers to optimal models of multidisciplinary approach to HF.
Annamaria Vianello
Gabriele Monasterio Foundation, Italy
Title: A case of misdiagnosed cardiomyopathy with rising plasma MMP9 long before sudden cardiac arrest
Time : 10:00-10:30

Biography:
Annamaria Vianello completed her Graduation at Medical School, Pisa University where she obtained Specialization both in Internal Medicine and in General Medicine. She completed her PhD in Medical Physiopathology and Pharmacology and in Normal and Pathological Morphology of Cells and Tissues; a second-level Short Specialization Degree in Clinical Pharmacological Research and; second-level Short Specialization Degree in Hypertrophic Cardiomyopathies at Pavia University. She worked as Fellow in Department of Internal Medicine and Sport Medicine, Pisa University. Her research interests include Athlete’s Heart Remodeling, Failing Heart Remodeling and Cardio-Renal Remodeling. She is currently coordinating a Tele-Health Project for out-of-hospital care of chronic heart failure. She is an Author of original papers dealing with the clinical role of circulating and tissue profiles of inflammatory biomarkers, MMPs and TIMPs in different models of heart remodeling such as Athlete’s Heart, Valvular Heart Disease, Cardio-Renal Failure and Chronic Heart Failure.
Abstract:
Introduction: Out-of-hospital cardiac arrest in the absence of structural heart disease is rare and can be due to subclinical cardiomyopathy or primary electrical disorders. Adverse collagen remodeling may occur in cardiac arrest patients; MMP-9 is proven to help risk stratification.
Clinical Case Description: In 2005, R.R, a 35 year old metal-worker, surprisingly began to show high values of MMP9. TIMPs, MMP2, NT-pro-BNP and all the other laboratory tests, abdominal echography, electrocardiogram and echocardiography were within the reference range. 10 years later, R.R suddenly collapsed at home; his wife promptly began a successful cardiac massage, supported by territorial tele-emergency network. R.R was admitted to the intensive unit with frequent ventricular extrasystoles, left ventricular dysfunction. Medical history of his family includes sudden death of two paternal uncles; mother with Takotsubo syndrome. Unremarkable clinical examination and electrocardiogram showed no biochemical evidence of acute myocardial infarction; CRP elevation. Un-obstructed coronary arteries on coronary were revealed in angiography. Chest X-ray showed mild interstitial fibrosis. There were no signs of arrhythmogenic cardiomyopathy on Cardio-NMR.
Discharge Diagnosis: Discharge diagnosis was: “Resuscitated cardiac arrest, in subject without evidence of structural heart disease, treated with ICD bicameral system”.
Reviewing Clinical Information & Diagnosis: Familial histories of sudden death, mild endocardial irregularities, left ventricle enlargement, reduced ejection fraction, low EKG voltage are suggestive of familial cardiomyopathy. Welding, chest X-ray fibrosis, RCP is suggestive of welder’s lung. Then, reformulated diagnosis: Resuscitated cardiac arrest in sub-clinical familial cardiomyopathy, chronically subjected to professional cardio-toxic damage.
Conclusions & Implications for Clinical Practice: R.R lethal arrhythmia was firstly considered as “idiopathic” in nature, since process laboratory and radiology testing were not analyzed properly. Interestingly, long before cardiac arrest, MMP9 had begun to rise, announcing a cardio-pulmonary adverse remodeling. The case of R.R teaches us that early biomarkers such as MMP9, correct and timely diagnosis, tele-medicine and emergency services network could really save lives of patients at high risk of sudden death.
Image:
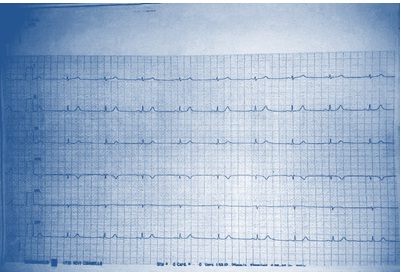
Figure 1: Low EKG voltage on peripheral leads
Prashant Tarakant Upasani
Metro Hospital & Heart Institute, India
Title: Advances in management of heart failure with emphasis on Angiotensin receptor neprilysin inhibitor (ARNI)
Time : 10:45:11:15

Biography:
Prashant Tarakant Upasani completed his DM (Cardiology) at All India Institute of Medical Sciences, New Delhi in May 1994. After completing his DM (Cardiology), he worked as Associate Consultant Cardiologist at Apollo Hospitals, Chennai and Indraprastha Apollo Hospitals, New Delhi. He is presently working at Metro Heart Institute, Noida as Senior Consultant Interventional Cardiologist. He is actively involved in all diagnostic and therapeutic interventional procedures. He was awarded Fellowship of College of Chest Physicians in the field of Pediatric Cardiology. In December 2012, he was conferred with Fellowship of Cardio-logical Society of India. He has 99 publications both in national and international journals including text books on cardiology. He has presented more than 80 papers in various national and international conferences. He is also the Coordinator of DNB Cardiology program at Metro Hospital, Noida.
Abstract:
Heart failure (HF) is an increasingly common syndrome associated with high mortality and economic burden. A range of terms has been used to describe HF viz. chronic HF (CHF), acute HF (AHF), HF with reduced ejection fraction (HFrEF) and HF with preserved ejection fraction (HFpEF). Pathophysiology of HFrEF is complex. Landmark trails in patient with HFrEF include SOLVD-T, CIBIS-II, CHARM-Alternative and CHARM-Added, SHIFT, EMPHASISHF and PARADIGM-HF. Natriuretic peptides (NPs) are a group of hormones that have potent effects on sodium and fluid balance. Neprilysin is a zinc-dependent metallopeptidase that catalyses the degradation of various peptides. Inhibition of neprilysin increases bioavailability of NPs, bradykinin, and substance P, resulting in natriuretic, vasodilatory and anti-proliferative effects. LCZ696 is useful not only for the treatment of HF but also likely to be a useful antihypertensive drug. LCZ696 is a novel drug that comprises sacubitril (AHU377) and valsartan in a 1:1 molar ratio. It simultaneously inhibits neprilysin and blocks AT1 receptors. PARADIGM-HF is the first study to test the efficacy of LCZ696 on morbidity and mortality in patients with HFrEF. The trail was stopped early, according to pre-specified rules, after a median follow-up of 27 months, because the boundary for an overwhelming benefit with LCZ696 had been crossed. LCZ696 was associated with a significantly lower death from cardiovascular causes or first hospitalization (taken together-20% or separately 20-21%). Secondary endpoint viz. death from any cause, showed a 16% reduction (p<0.001). The superiority of LCZ696 over enalapril was not accompanied by important safety concerns. The LCZ696 group had a higher proportion of patients with non-serious angioedema, but not associated with an increase in serious angioedema.

Biography:
Vladimir Ermoshkin completed his Graduation in Physics department at Moscow State University in 1978. He has worked at Russian New University (RosNOU) as Physicist. He has published 10 articles on Cardiology in prominent magazines (Russian and English).
Abstract:
Aim:C делана попытка нового анализа м еханизм а An attempt to study the mechanism of heart failure.
Method: Information search in the literature, participate in conferences, discussions with Russian leading cardiologists.
Result: Having heart failure means that for some reason your heart is not pumping blood around the body as well as it used to. Heart failure can be a major manifestation of virtually all diseases of the heart, including coronary atherosclerosis, myocardial infarction, acquired valvular disease, congenital heart disease, arrhythmias and cardiomyopathy. Populationâ€based echocardiographic studies have demonstrated that more than 50% of participants with left ventricular systolic dysfunction (generally defined as LVEF <35–40%) have no symptoms or signs of heart failure. How to interpret this data? How the heart can pump insufficient blood to one person and sufficient amount of blood to another? Where is the logic? The reason according to my theory of CVD is that, near liver, arteriovenous anastomoses (AVA) or cascade AVA opens for longer time than optimal. Veins overflow begin mechano-induced arrhythmia. Opened AVA lead to stagnation of blood in the area of small pelvis and ankle/feet. The other reasons are stasis of microcirculations, weight gain, varicose veins, endometriosis, prostatitis, hemorrhoids, thrombosis, and cancer. The development of these diseases is accompanied in most cases with heart failure.
Conclusions: It is necessary to correct the glaring errors in cardiology which are existing from past 50-100 years. It is necessary to develop pulse wave suppressors and artificial anastomosis with an adjustable diameter hole.
Josephine Achan
Uganda Heart Institute, Uganda
Title: Clinical presentation and in-hospital outcome of patients with myocardial infarction admitted in Mulago hospital

Biography:
Josephine Achan is a young Researcher with special interest in Cardiovascular Disease. She is currently practicing at Uganda Heart Institute as a Physician and a second year adult Cardiology Fellow. She is involved in the local research in her country and currently part of Acute Myocardial Infarction in Uganda.
Abstract:
Introduction: Myocardial infarction is one of the leading causes of mortality worldwide with decreasing incidence in developed countries and increasing incidences in developing countries, Uganda inclusive. This increasing trend has been attributed to urbanization and changing life styles in developing countries. There is high burden of risk factors like hypertension and diabetes mellitus in our setting.
Aim: The purpose of this study is to describe the clinical presentation and in-hospital outcome among patients admitted with myocardial infarction at Mulago Hospital.
Method: This was a prospective cohort study that was conducted in Mulago Hospital complex and Uganda Heart Institute in 2013. 54 subjects were recruited during the eight months study period. Data collected through standardized questionnaire and blood samples obtained. Participants were followed for minimum of two weeks and maximum of one month.
Results: A total of 54 patients were recruited, 29/54 (63%) had ST segment elevation myocardial infarction (STEMI) and 17/54 (37%) had non-ST segment elevation myocardial infarction. Chest pain (66.7%) was the common presentation. Most patients in this study came to the hospital more than 72 hours with median time of presentation to the hospital from onset of symptoms 93.5 hours (SD 57.09, OR=1.002 95% CI 0.9-1.0). The mean age for the study participants was 58.7 (SD=+/-10) with more males 38/54 (70.4%) than females 16/54 (29.6%). Common associated symptoms were breathlessness 39/54 (54.7%), palpitations 21/54 (38.9%). Symptoms occurred at rest with exercise and emotional stress. Only 7/59 (13%) of the participants had low systolic and 11/54 (20.4%) low diastolic blood pressure. 18/54 (33.3%) had high systolic and 20/54 (37%) diastolic pressure at admission. 19/54 (35.2%) of participants had significant pulmonary rales at admission. 34/54 (63%) had New York Heart Association class I and 40/54(74.1%) were in Killip class I. Risk factors included past medical history of hypertension 35/54 (OR=1.53, 95% CI=0.48-4.90), diabetes mellitus (OR=1.52, 95% CI=0.46-4.95), dyslipidemia 7/54 (OR=1.73, 95.5 CI=0.29-10.10), high LDL cholesterol were higher risk for myocardial infarction. Low HDL (OR=1.9, 95% CI=0.55-6.58) confers higher risk for myocardial infarction compared to normal and high HDL cholesterol levels. Also similar patterns were seen in family history as positive for hypertension (59.3%) (OR=1.1, 95.5 CI=0.35-3.88) and diabetes mellitus (37%). Overall 10/54 (24.1%) developed shock, 10/54 (18.5%) had pulmonary oedema and congestive heart failure, 6/54 (11.1%) developed arrhythmia, 6/54 (11.1%) died in the hospital, and 2/54 (3.7%) had ventricular wall aneurysm formation. 1/54(1.9%) had stroke, reinfarction and thrombus formation.
Conclusion: Majority of patients admitted with myocardial infarction had STEMI and presented with chest pain. Most patients were males. Hypertension, diabetes mellitus and dyslipidemia were high risk factors. Almost half of the patients with STEMI developed pulmonary edema, shock, congestive heart failure and arrhythmia.
Rhodaline Yayra Odoi
V.N. Karazin National University, Ukraine
Title: Obesity and the heart: Obesity management
Time : 11:45-12:15

Biography:
Rhodaline Yayra Odoi is a second-year Medical student at V.N. Karazin National University, Ukraine where she is currently pursuing General Medicine. She is looking forward to specialize in Pediatrics/Gynecology and Obstetrics after medical school. She has previously volunteered at Tema General Hospital (Tema-Ghana), Korle-Bu Teaching Hospital (Accra-Ghana), where she worked at the Pediatrics and Gynecology and Obstetrics department. She is looking forward to work with Hamad General hospital (Doha, Qatar).
Abstract:
Statement of the Problem: Obesity which is excess fatty weight is one of the most predominant cardiovascular risk factor. The association between obesity and cardiovascular disease is complex and not limited to the standard risk factors like hypertension, dyslipidemia, and type 2 diabetes mellitus. Recent years researches have shown that obesity causes most cardiovascular diseases through mechanisms like subclinical inflammation, endothelial dysfunction, increased sympathetic tone, atherogenic lipid profiles, enhanced thrombogenic factors, and also through obstructive sleep apnea. The purpose of this study is to create awareness of obesity, its bad outcome and to awaken us on the lifestyle we live.
Methodological & Theoretical Orientation: Based on my research done in Ghana, people with issues of obesity have cardiovascular disease.
Findings: Several studies have shown association between obesity and prognosis among those with coronary disease and heart failure, this may be due to limitations of ways we define obesity. There are numerous data suggesting that measuring central obesity or total body fat content might be more appropriate than using the body mass index method alone.
Conclusion: The management of obesity is challenging and studies using lifestyle modification alone or with pharmacologic agents generally have limited success and high levels of weight regain. Bariatric surgery has proven to be an effective and safe way to induce and maintain significant weight loss but its limited to those with medically complicated obesity or people who are severely obese therefore urging imminent doctors and medical practitioners to thoroughly educate their patients who are obese or yet to get obese on the bad effect of obesity and also encourage them to exercise regularly which may reduce their weight and also help boost their metabolic activities hence keeping them healthy.
Image:
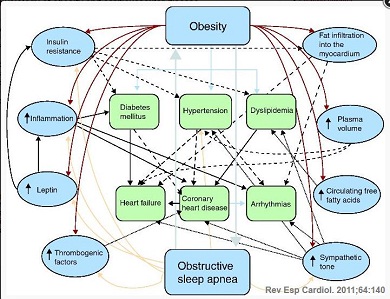
Figure 1: Pathophysiology of obesity and cardiovascular disease.
Umme Habiba Ferdaushi
National Institute of Cardiovascular Diseases (NICVD), Bangladesh
Title: Short term outcome of cardiac resynchronization therapy on functional recovery of patients with congestive heart failure in Bangladeshi population
Time : 12:15-12:45

Biography:
Umme Habiba Ferdaushi has completed her MBBS at Shere Bangla Medical College, Barisal, Bangladesh and fellowship in Cardiology at Bangladesh College of Physicians and Surgeons (BCPS), Bangladesh. She works at National Institute of Cardiovascular Diseases (NICVD), a tertiary level cardiovascular institute. She has published three papers in reputed journals.
Abstract:
Background & Aim: Cardiac resynchronization therapy (CRT) reduces symptoms and improves left ventricular function in patients with heart failure due to left ventricular systolic dysfunction and cardiac dyssynchrony. We analyzed the clinical and echocardiographic outcome of CRT in heart failure patients.
Methods: A total 35 heart failure patients were included in this prospective observational study, conducted from Feb 2015–Feb 2016 in the cardiology department of NICVD, Dhaka. Demographic profile, clinical data and investigations including coronary angiogram were done. Patients underwent CRT-P (BiV pacemaker) or CRT-D (defibrillator) and were followed up. Clinical, electrocardiographic and echocardiographic study were performed before and three months after CRT implantation.
Results: After three months of BiV pacing, New York Heart Association functional class improved from 3.3±0.44 to 1.7±0.6 (p<0.001). Left ventricular end diastolic diameter was reduced from 67.9±5.2 to 61.9±5.9 mm (p<0.001) and left ventricular end systolic diameter was reduced from 56.4±6.5 to 50.5±7.2 mm (p<0.001). Ejection fraction was significantly increased after three months from 27.5±4.3% to 38.8±6.7%, (p<0.001).The average grade of mitral regurgitation was decreased from 1.49±0.65 to 0.43±0.61 (p<0.001). The number of hospitalization was also significantly reduced from 2.51±1.44 to 0.11±0.32 (p<0.001). Among the study patients, 71.4% patient was responders, 17.1% super responders and 11.4% non-responders.
Conclusions: Although the study was performed on a small number of patients, it can be considered that CRT had favorable hemodynamic and clinical results and reduced the need for hospitalization in our heart failure patients.
Wei Hua
Fuwai Hospital & Cardiovascular Institute, China
Title: The clinical outcome of cardiac resynchronization therapy in dilated-phase hypertrophic cardiomyopathy

Biography:
Wei Hua is a Professor of Cardiology, Deputy Director at Cardiac Arrhythmia Center, Fuwai Hospital & Cardiovascular Institute, Chinese Academy of Medical Sciences, Peking Union Medical College, China. He completed his MD at Shanghai Medical University in 1985 and then PhD at Graduate School of Peking Union Medical College. He joined Fuwai Hospital & Cardiovascular Institute in 1985 and became full Professor of Cardiology in 1999. He was trained in Cardiac Pacing and Electrophysiology in Royal Melbourne Hospital, Australia, from 1994-1996. His main work is on “Clinical cardiac pacing and electrophysiology, cardiac arrhythmias service”. He is now Vice Chairman of Chinese Society of Pacing and Electrophysiology (CSPE) and Chairman of Cardiac Pacing Committee of CSPE. He is a Fellow of Heart Rhythm Society (FHRS), European Heart Rhythm Association (EHRA) and New York Academy of Sciences.
Abstract:
Statement of the Problem: Clinical trials have demonstrated that cardiac resynchronization therapy (CRT) is effective in patients with non-ischemic cardiomyopathy. However, patients with dilated-phase hypertrophic cardiomyopathy (DHCM) have been generally excluded from such trials. We aimed to compare the clinical outcome of CRT in patients with DHCM, idiopathic dilated cardiomyopathy (IDCM) or ischemic cardiomyopathy (ICM).
Methodology & Theoretical Orientation: A total of 312 consecutive patients (DHCM=16; IDCM=231; ICM=65) undergoing CRT in Fuwai hospital were studied respectively. Response to CRT was defined as reduction in left ventricular end-systolic volume (LVESV) ≥15% at six-month follow-up.
Findings: Compared with DHCM, IDCM was associated with a lower total mortality [hazards ratio, HR: 0.35 (95% confidence interval, CI 0.13-0.90)], cardiac mortality [HR: 0.29 (95% CI 0.11-0.77)] and total mortality or heart failure (HF) hospitalizations [HR: 0.34 (95% CI 0.17-0.69)], independent of known confounders. Compared with DHCM, the total mortality, cardiac mortality and total mortality or HF hospitalizations favored ICM but were not statistically significant. [HR: 0.59 (95% CI 0.22-1.61); HR: 0.59 (95% CI 0.21-1.63); HR: 0.54 (95% CI 0.26–1.15) respectively]. Response rate to CRT was lower in the DHCM group than the other two groups although the differences didn't reach statistical significance.
Conclusion & Significance: Compared with IDCM, DHCM was associated with a worse outcome after CRT; the clinical outcome of DHCM patients receiving CRT was similar to or even worse than that of ICM patients. These indicate that DHCM behaves very differently after CRT.
Biography:
Vladimir Ermoshkin completed his Graduation in Physics department at Moscow State University in 1978. He has worked at Russian New University (RosNOU) as Physicist. He has published 10 articles on Cardiology in prominent magazines (Russian and English).
